Our Science
MAXIMIZING THE POWER OF MELANOCORTIN AGONISTS
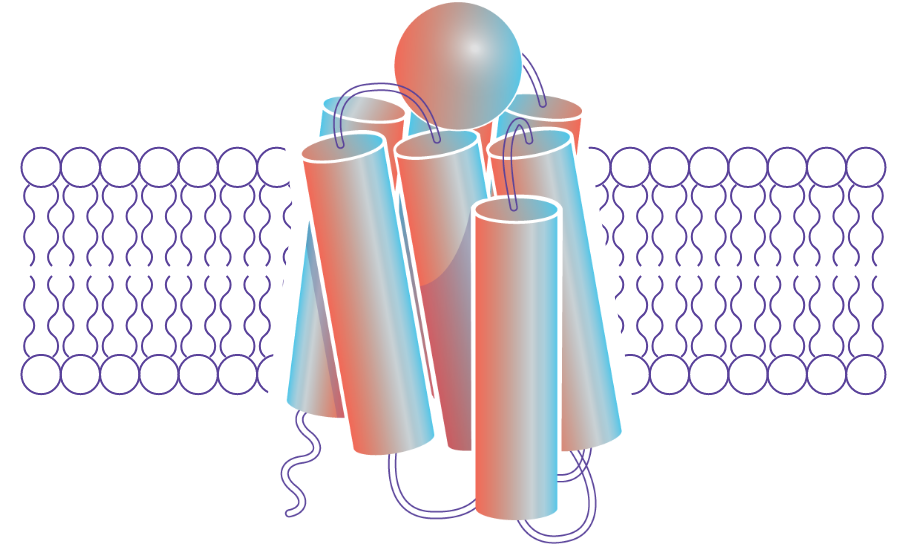
The melanocortin system is mediated by a family of five related receptors that are essential to the body’s control of inflammation, immune response, metabolism, steroid hormone production, and sexual function. This expansive range of effects can be targeted by Palatin’s receptor-selective drugs.
View our science video
Harnessing the Melanocortin System in the Body
Brain
Melanocortin receptors found in the hypothalamus regulate weight maintenance and sexual function, allowing therapeutic interventions that can help people take back control.EYES
Many tissues and immune cells located in the eye express melanocortin receptors, empowering the opportunity to directly activate natural pathways to resolve disease-associated inflammation.Colon
Locally engaging melanocortin receptors found in the intestinal lining and immune cells provides a novel approach to reducing bowel inflammation.Kidney
Kidney cells important to its function express the melanocortin receptor 1 (MCR1). Activating these receptors may improve kidney function and health in a variety of kidney diseases.
We research, design, and develop novel highly selective peptides and small molecule agonists targeted for specific melanocortin receptors.
Our current focus is on the design and development of receptor selective melanocortin agonists for inflammation and autoimmune conditions, with a focus on ocular diseases. Our therapeutics work by activating endogenous melanocortin pathways to resolve damaging inflammation and allow affected tissues time to heal. Research has shown melanocortin agonists can prevent and reverse inflammation in disease models, including in the eyes and intestine—two of our targeted areas.
ADVANCING THE TREATMENT OF OCULAR DISEASES
Currently available ocular drugs are hindered by adverse side effects, including poor efficacy, high discontinuation rates, and slow onset of action. Together, these factors create a suboptimal experience, leading to frustration and a need for effective interventions.
Melanocortin receptors are present on the surface of many different cells in the eye, as well as in immune cells residing in the ocular tissue. These melanocortin receptors are a highly tractable target for melanocortin agonists to provide relief and healing for those living with ocular diseases.
LEADING THE WAY IN THE TREATMENT OF AUTOIMMUNE DISEASES
Current treatments for inflammation and autoimmune diseases, such as steroids, immune system modulators, and biologics, broadly suppress immune response. These approaches can impair the body’s immune capabilities on a systemic level, causing adverse side effects and safety concerns.
Melanocortin agonists can potentially resolve inflammation and avoid the adverse side effects and safety concerns of immunosuppressants.
The intestinal lining and resident immune cells express MCR1, and preclinical disease models demonstrate that these receptors can play an important role in controlling colonic inflammation present in ulcerative colitis (UC). Local administration via oral dosing allows our melanocortin agonist to interact with the receptors found on the apical surface of the colon and avoid systemic absorption, and therefore, any associated concerns.
EXTENSIVE CLINICAL PIPELINE
Find out how we continue to leverage our melanocortin agonist expertise to address the unmet needs of patients living with inflammatory and autoimmune diseases.